Urinary tract infections in ostomates: a subtle connection between the three microbiomes
Having an operation can be an emotionally charged time, full of anxiety. Things that you took for granted may now require a bit more attention and effort. You have to watch out for skin irritation or signs of infection after a colostomy or ileostomy as well as drink plenty of water to avoid dehydration, eat those foods that agree with you and don’t cause excess wind or an increased output. You have to retrain your digestive system to cope with normal foods that you used to enjoy before you had a stoma.
Another potential problem that may arise is frequent urinary tract infections, even if you were not prone to them previously. You could also experience episodes of vaginal thrush. UTIs and thrush are irritating and uncomfortable, and it is not always obvious why they occur when your hygiene is really good.
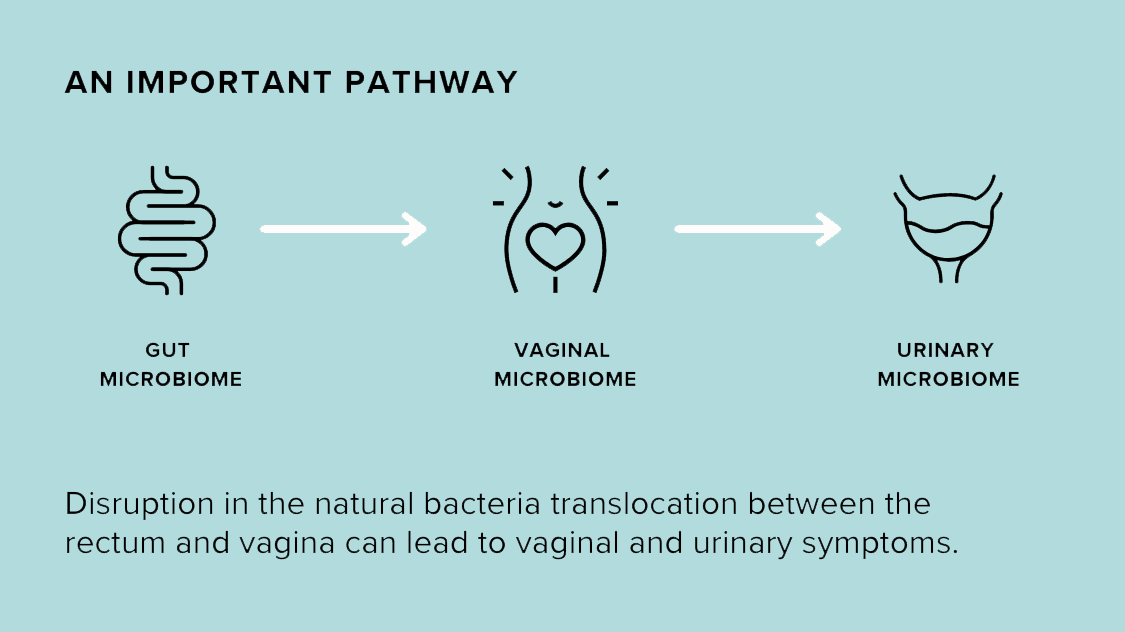
It is only human to zoom in on the main presenting problem, forgetting about the wider picture and the fact that everything in the body is inter-connected and nothing happens in isolation. The human body hosts three distinct but interconnected bacterial microbiomes in the lower region: the gut microbiome, the vaginal microbiome (in women) or the prostate/seminal fluid microbiome (in men), and the urinary microbiome (including the bladder). While the bladder and urine were once thought to be sterile, recent studies have revealed the existence of the urinary microbiome and its interplay with the other two. These communities are not isolated; they communicate and interact with each other, even with variations in hygiene practices.
Low count but diverse microbial communities were discovered in urine, and instead of being viewed as unwelcome intruders causing problems, it is now suggested that they may maintain normal bladder homeostasis and play a protective role against infections.
The Three Microbiomes and Their Interconnection
Where do these bacteria come from? Well, most of our gut bacteria came from our mothers after we went through the birth canal during birth. For babies born via Caesarian section, the primary source of gut microbiome is breast milk and skin contact with their mothers. While C-section babies receive fewer microbes from their mother's gut during birth compared to vaginally delivered babies, they are able to compensate for this through the microbes present in breast milk. Exclusive breastfeeding for at least six months is recommended for C-section babies to help their gut microbiota shift towards a profile similar to vaginally delivered infants.
The vaginal microbiome is largely derived from the gut microbiome, but because the ‘living conditions’ in the vagina are different, different species of bacteria survive and thrive there. These mainly include various types of Lactobacilli, which create a protective slightly acidic environment. It plays a crucial role in maintaining vaginal health. A healthy vaginal pH typically ranges from 3.8 to 4.5. This acidic environment helps to protect against harmful bacteria and yeast overgrowth, which can lead to infections. Other bacterial species may be introduced during intercourse with your sexual partner, and you start sharing your microbiomes to some extent.
The relationship, between the lesser-known semen microbiome and the gut microbiome is unclear at present and needs more research, but experts have a few theories. Dr. Menka Gupta, a functional medicine doctor with NutraNourish, tends to think that it may be possible to improve semen microbiome health by improving gut health. He can see a potential connection between the gut and the semen microbiome through diet, level of stress and exposure to toxins.
The urinary microbiome is now known to originate primarily from the gut and the vagina in women. In men, semen and urine both travel through the urethra, but they are separated by a sphincter muscle that prevents them from mixing. Even though they don’t pass through this channel at the same time, they share the same route and therefore it is possible that the pathogenic bacteria that causes prostatitis, for example, could travel up the urethra causing a UTI and could even penetrate the urinary bladder, and vice versa. In a similar way, beneficial and protective bacteria could be shared between the seminal fluid and the urinary tract. At this point in time the gut and vaginal microbiomes are considered the main source of both pathogenic and beneficial bacteria for the urinary microbiome, depending on their specific composition.
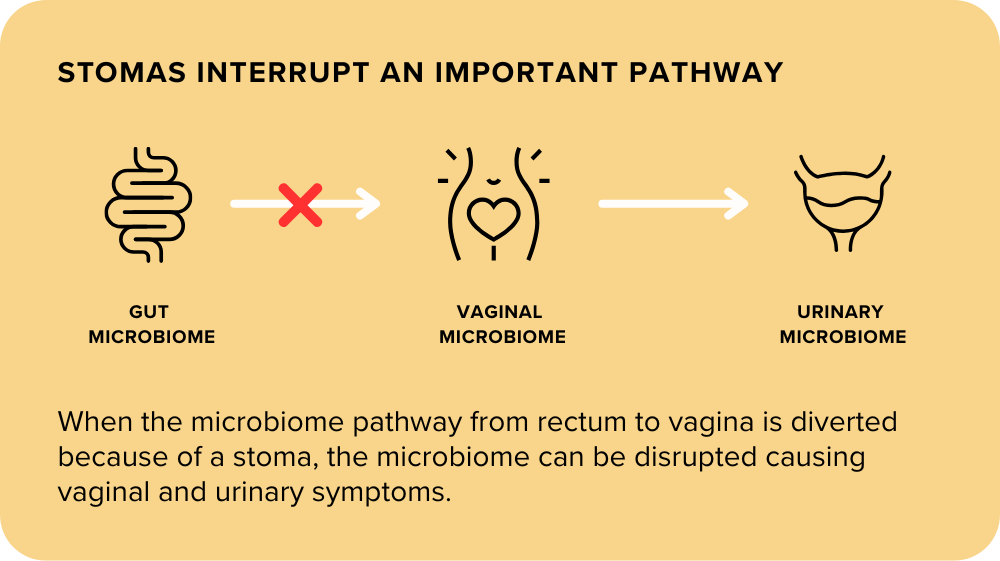
It is clear that the gut microbiome plays the leading role in ‘reseeding’ the good protective bacteria both in the vagina and the urinary tract. When this natural door of bacterial translocation is shut due to surgery, vaginal and urinary problems may arise.
The natural bacterial exchange between these three microbiomes becomes interrupted after a stoma is created. If you experience frequent UTIs, thrush or vaginal irritation after an ileostomy or colostomy and find that oral supplementation of probiotics does not help any more, try a local application of probiotics. The direct route seems to work more effectively in this situation.
Leslie Mello from Colostomy UK interviewed me on the subject for an article in Tidings Magazine. For the full article please click here.
References
Science Direct Article on infant microbiome
https://www.medicalnewstoday.com/articles/semen-microbiome-linked-to-male-infertility
© Marina Townsley, ND
Master Herbalist AMH, Nutritional Therapist BANT